Stapled Hemorrhoidopexy: A Modern Approach to Treating Hemorrhoids
Introduction:
Hemorrhoids, a condition that affects millions of people worldwide, can be a source of discomfort, pain, and embarrassment. Fortunately, medical advancements have led to various treatment options, including the innovative technique known as Stapled Hemorrhoidopexy. In this comprehensive guide, we'll delve into the details of Stapled Hemorrhoidopexy, exploring its benefits, procedure, recovery, and potential complications.
Understanding Hemorrhoids:
Hemorrhoids are swollen blood vessels located in the rectum and anus, causing symptoms like itching, bleeding, pain, and discomfort during bowel movements. Factors such as a sedentary lifestyle, poor dietary habits, pregnancy, and chronic constipation can contribute to the development of hemorrhoids.
The Evolution of Hemorrhoid Treatment:
Historically, surgical intervention for hemorrhoids involved excision or ligation, which could be painful and require significant recovery time. However, medical progress has led to the development of minimally invasive procedures like Stapled Hemorrhoidopexy.
Stapled Hemorrhoidopexy Explained:
Stapled Hemorrhoidopexy, also known as Procedure for Prolapse and Hemorrhoids (PPH), is a modern surgical technique designed to treat advanced internal hemorrhoids. This procedure aims to correct the anatomical abnormalities that contribute to hemorrhoid development, providing long-term relief to patients.
The Procedure:
1. Preparation: Before the surgery, patients undergo thorough evaluation, including medical history and physical examination, to ensure they are suitable candidates for Stapled Hemorrhoidopexy.
2. Anesthesia: The procedure is usually performed under general anesthesia or spinal anesthesia, ensuring the patient's comfort and safety.
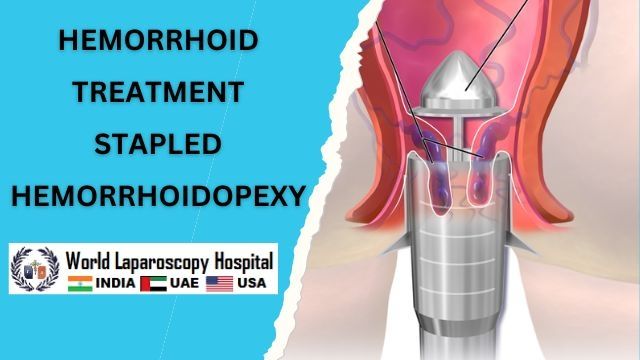
3. Surgical Steps: The surgeon employs a circular stapler device to reposition the hemorrhoids and restore their normal blood flow. This involves removing excess tissue and pulling the hemorrhoidal cushions back into their proper position.
4. Stapling: The circular stapler simultaneously excises the excess tissue and restores the hemorrhoidal cushions, reducing their prolapse and blood supply issues.
5. Closure: The procedure results in a circular staple line, promoting the healing of the affected area.
Benefits of Stapled Hemorrhoidopexy:
1. Minimally Invasive: Stapled Hemorrhoidopexy is less invasive than traditional surgical methods, resulting in shorter recovery times and less post-operative discomfort.
2. Reduced Pain: Patients typically experience less pain and discomfort after the procedure compared to conventional surgeries.
3. Faster Recovery: The minimally invasive nature of Stapled Hemorrhoidopexy allows patients to return to their normal activities sooner.
4. Lower Risk of Complications: Stapled Hemorrhoidopexy carries a lower risk of infection and wound-related complications compared to traditional surgical approaches.
Recovery and Aftercare:
Following the procedure, patients are provided with detailed instructions for post-operative care. This may include dietary recommendations, pain management strategies, and guidance on maintaining proper hygiene. While recovery times vary, many individuals can expect to resume their daily routines within a few days to a week after surgery.
Potential Complications:
While Stapled Hemorrhoidopexy is generally safe and effective, as with any medical procedure, there are potential risks and complications. These may include bleeding, infection, recurrence of hemorrhoids, or rare instances of damage to nearby structures. Patients should promptly report any unusual symptoms or concerns to their healthcare provider.
Risks and Benefits of Stapled Hemorrhoidopexy: A Comprehensive Analysis
Hemorrhoids, a common medical condition, can significantly impact an individual's quality of life. Among the various treatment options available, Stapled Hemorrhoidopexy has emerged as a promising and innovative approach. In this extended exploration, we will delve deeper into the risks and benefits of Stapled Hemorrhoidopexy, shedding light on its potential advantages and considerations.
Benefits of Stapled Hemorrhoidopexy (PPH):
1. Reduced Pain and Discomfort: One of the most significant advantages of Stapled Hemorrhoidopexy is the potential for reduced post-operative pain and discomfort. Unlike traditional hemorrhoidectomy procedures, which involve the excision of tissue, stapling focuses on restoring the normal anatomical position of the hemorrhoidal cushions. This results in less trauma to the surrounding tissues and nerves, leading to a more comfortable recovery period.
2. Minimally Invasive Approach: Stapled Hemorrhoidopexy is considered a minimally invasive technique. The procedure is performed using specialized instruments and a circular stapler device, which reduces the need for extensive incisions. This approach not only decreases the risk of infection but also contributes to shorter hospital stays and quicker recovery times.
3. Faster Recovery: Individuals who undergo Stapled Hemorrhoidopexy typically experience a faster recovery period compared to traditional surgical methods. Many patients can resume their daily activities, including work and exercise, within a relatively short period after the procedure. This allows for a quicker return to normal life and routine.
4. Minimal Risk of Anal Stenosis: Anal stenosis, a potential complication of traditional hemorrhoidectomy, is less likely to occur with Stapled Hemorrhoidopexy. The circular stapling technique preserves the natural anatomical structure of the anal canal, reducing the risk of narrowing and potential complications associated with bowel movements.
Risks and Considerations:
1. Risk of Recurrence: While Stapled Hemorrhoidopexy has shown success in treating hemorrhoids, there is still a possibility of recurrence over time. As with any medical procedure, individual factors, such as lifestyle and underlying medical conditions, can influence the long-term outcome.
2. Potential Complications: Although Stapled Hemorrhoidopexy is generally considered safe, there are potential risks associated with the procedure. These may include bleeding, infection, and rare instances of damage to surrounding structures. Patients should be aware of these potential complications and promptly report any concerning symptoms to their healthcare provider.
3. Patient Selection: Not all individuals with hemorrhoids are suitable candidates for Stapled Hemorrhoidopexy. The procedure is typically recommended for patients with internal hemorrhoids that have prolapsed or are causing significant discomfort. A thorough evaluation by a qualified healthcare professional is essential to determine the most appropriate treatment approach for each patient.
4. Cost Considerations: While the benefits of Stapled Hemorrhoidopexy are evident, it's important to consider the potential costs associated with the procedure. Depending on factors such as insurance coverage and geographical location, the financial aspect of the treatment should be discussed with the healthcare provider.
Performing Stapled Hemorrhoidopexy: A Step-by-Step Guide to Surgical Technique
Stapled Hemorrhoidopexy, also known as Procedure for Prolapse and Hemorrhoids (PPH), is a modern and minimally invasive surgical technique designed to treat advanced internal hemorrhoids. This innovative procedure focuses on repositioning the hemorrhoidal cushions and correcting the underlying anatomical issues that contribute to hemorrhoid development. Below, we provide a detailed step-by-step guide to performing Stapled Hemorrhoidopexy.
Preoperative Preparation:
1. Patient Evaluation: Begin by conducting a thorough evaluation of the patient's medical history, physical condition, and hemorrhoid severity. Ensure that the patient is an appropriate candidate for Stapled Hemorrhoidopexy based on the extent of prolapse and other relevant factors.
2. Anesthesia: Administer general anesthesia or spinal anesthesia to ensure the patient's comfort and minimize pain during the procedure.
1. Patient Positioning: Position the patient in lithotomy (lying on their back with legs elevated and flexed) or prone position to provide optimal access to the surgical site.
2. Speculum Insertion: Insert a specialized anal dilator or proctoscope to gain clear visibility and access to the anal canal and rectum.
3. Circumferential Dissection: Use blunt dissection to create a circumferential plane just above the dentate line, separating the hemorrhoidal cushions from the underlying tissue. This step helps to free the hemorrhoidal tissue for repositioning.
4. Hemorrhoidal Prolapse: Gently pull down the prolapsed hemorrhoidal cushions into the anal canal using atraumatic instruments. This step is crucial for achieving proper repositioning.
5. Stapler Insertion: Insert a circular stapling device through the anus and into the anal canal, ensuring that the hemorrhoidal cushions are properly positioned within the stapler's circular cartridge.
6. Stapling and Tissue Resection: Activate the stapling device, which simultaneously excises excess hemorrhoidal tissue and restores the hemorrhoidal cushions to their anatomically correct position. The device places a circular row of staples above the dentate line.
7. Closure and Healing: As the stapler is activated, it creates a circular staple line, effectively closing the wound. This minimizes bleeding and promotes healing of the repositioned hemorrhoidal tissue.
8. Stapler Removal: Carefully withdraw the stapling device, ensuring that the repositioned hemorrhoidal tissue remains intact.
Postoperative Care:
1. Pain Management: Provide appropriate pain management medication to ensure the patient's comfort during the initial stages of recovery.
2. Diet and Hygiene: Instruct the patient on post-operative dietary restrictions and hygiene practices to prevent infection and promote healing.
3. Activity and Recovery: Advise the patient on resuming normal activities, gradually increasing physical activity as tolerated, and avoiding strenuous activities during the initial recovery period.
4. Follow-Up: Schedule follow-up appointments to monitor the patient's healing progress and address any concerns or complications that may arise.
Potential Complications and Considerations:
1. Bleeding: Monitor the patient for post-operative bleeding, which is a potential complication. Instruct the patient to report any significant bleeding or changes in bowel habits.
2. Infection: Emphasize the importance of proper hygiene and wound care to minimize the risk of infection.
3. Recurrence: While Stapled Hemorrhoidopexy is effective, educate the patient about the possibility of recurrence over time and the importance of maintaining a healthy lifestyle.
Stapled Hemorrhoidopexy is a sophisticated surgical technique that requires skill, precision, and a comprehensive understanding of the underlying anatomy. Surgeons who perform this procedure must be well-trained and experienced to ensure successful outcomes and minimize the risk of complications. By following the step-by-step guide outlined above and considering potential complications, healthcare professionals can provide patients with a promising option for treating advanced internal hemorrhoids and enhancing their overall quality of life.
Advantages of Laparoscopic Stapled Hemorrhoidopexy: Enhancing Hemorrhoid Surgery with Minimally Invasive Techniques
Laparoscopic Stapled Hemorrhoidopexy, a variation of the traditional Stapled Hemorrhoidopexy (PPH) procedure, combines the benefits of both laparoscopic surgery and the innovative stapling technique to treat advanced internal hemorrhoids. This advanced approach offers several advantages over open surgical methods, making it a preferred choice for many patients and healthcare providers. In this article, we will delve into the advantages of performing Stapled Hemorrhoidopexy through laparoscopy.
Laparoscopic surgery involves making small incisions through which specialized instruments and a tiny camera (laparoscope) are inserted. This technique offers distinct advantages over open surgery, including:
1. Reduced Trauma: Laparoscopic Stapled Hemorrhoidopexy involves smaller incisions, leading to less trauma to surrounding tissues, reduced blood loss, and minimal scarring.
2. Faster Recovery: Patients who undergo laparoscopic surgery typically experience shorter hospital stays and quicker recovery times compared to open surgery. This allows them to return to their normal activities sooner.
3. Less Postoperative Pain: Smaller incisions and reduced tissue manipulation lead to less postoperative pain, enabling patients to manage discomfort more effectively.
Advantages Specific to Laparoscopic Stapled Hemorrhoidopexy:
1. Enhanced Visualization: The laparoscope provides a magnified, high-definition view of the surgical site, allowing for precise manipulation and accurate stapling. Surgeons can clearly assess the extent of hemorrhoidal prolapse and make informed decisions during the procedure.
2. Better Stapler Placement: Laparoscopic stapling allows for precise positioning of the circular stapler device, ensuring optimal closure and repositioning of the hemorrhoidal cushions. This contributes to a more successful outcome and reduces the risk of complications.
3. Reduced Tissue Handling: Laparoscopic techniques involve less tissue manipulation, leading to reduced trauma to the anal canal and surrounding structures. This minimizes the risk of postoperative discomfort, anal stenosis, and other complications.
4. Lower Risk of Infection: Smaller incisions and reduced tissue exposure can lead to a decreased risk of surgical site infections, promoting better overall outcomes.
5. Customized Approach: Laparoscopic Stapled Hemorrhoidopexy allows the surgeon to tailor the procedure to the patient's specific needs. The surgeon can address individual variations in hemorrhoid anatomy, ensuring the best possible outcome.
Conclusion:
Stapled Hemorrhoidopexy represents a significant advancement in the treatment of hemorrhoids, offering a minimally invasive approach with several benefits over traditional surgical methods. This modern technique has the potential to provide lasting relief from the discomfort and inconvenience caused by hemorrhoids, allowing individuals to regain their quality of life and overall well-being.
As with any medical procedure, it's essential to consult with a qualified healthcare professional to determine if Stapled Hemorrhoidopexy is the right choice for your individual circumstances. If you're suffering from hemorrhoids, don't hesitate to explore the possibilities that this innovative procedure has to offer. Your journey toward improved comfort and relief may begin with the transformative approach of Stapled Hemorrhoidopexy.
Comments
Post a Comment